Apr 15, 2013 | PRP, Research, Staff Articles
Abstract
OBJECTIVE: The purpose of this article is to detail the biology of platelet-rich plasma (PRP), critically review the existing literature, and discuss future research applications needed to adopt PRP as a mainstay treatment method for common musculoskeletal injuries.
CONCLUSION: Any promising minimally invasive therapy such as PRP deserves further investigation to avoid surgery. Diagnostic imaging outcome assessments, including ultrasound-guided needle precision, should be included in future investigations.
KEYWORDS: musculoskeletal imaging • platelet-rich plasma • tendinopathy • ultrasound
Introduction
Chronic musculoskeletal injuries involving tendon, muscle, ligament, and bone have long eluded the use of standardized therapeutic protocols, regardless of cause. Ultrasound-guided fenestration or tenotomy has been used with success as a potential treatment of chronic tendinopathies. In addition, researchers have tested the efficacy of a wide array of injectable agents, from relatively simple solutions such as hyperosmolar dextrose (prolotherapy) to complex orthobiologic agents such as bone morphogenic protein, but none have met with uniform success. Plateletrich plasma (PRP) injection has emerged as a treatment alternative for many musculoskeletal conditions. Although concentrated platelet therapy, which includes PRP, has been used for 20 years, it has recently been popularized by the media after its positive effects were reported to be responsible for an American professional football player’s accelerated return to play and subsequent victory in the 2009 Super Bowl.
PRP is defined as a platelet concentration higher than the physiologic platelet concentration found in healthy whole blood. Some authors have adopted a more objective definition of five times the platelet concentration of whole blood. The ability to concentrate platelets allows a higher concentration of the bioactive growth factors reported to promote healing. There are currently many clinical applications of PRP, including bone healing in oral maxillofacial surgery, postoperative wound healing, and postoperative rotator cuff repair integrity in orthopedic surgery. The positive effects in these intraoperative applications have stimulated the use of PRP in the sports medicine outpatient clinic setting, mostly for chronic tendinopathies and often in a collaborative setting involving a musculoskeletal radiologist who assists in diagnosis, imaging-guided injection of PRP, and follow-up. The recent explosion of the clinical use of PRP has outpaced evidence-based research. Few randomized controlled studies and smaller anecdotal case reports document clinical success of PRP. This article will detail the biology of PRP, critically review the existing efficacy studies, and discuss future research applications that need to be performed if PRP is to be adopted as a mainstay treatment method for common musculoskeletal injuries.
Biology of PRP
The average platelet concentration of whole blood is 200,000 per µL (normal range 150,000–350,000 per µL). Platelets are small anucleated cytoplasmic fragments of megakaryocytes that are commonly thought of as the responsible agents for hemostasis. Although the platelet is central to the coagulation cascade, it is also essential to tissue healing. The first step of the healing process is clot formation and platelet activation. After platelet activation, many growth and differentiation factors are released from the -granules, which are storage units found in platelets. Ninety-five percent of the existing factors are released within 10 minutes of clot formation, whereas the rest of the growth factors are released as they are formed over several days. In vivo and in vitro research also suggest that PRP induces overexpression of additional endogenous growth factors beyond what is contained within the platelet concentrate.
Wound healing involves an intricate process that is often categorized into three overlapping phases: inflammation, proliferation, and remodeling. Once tissue injury occurs, a hematoma forms at the site of tissue damage, platelets adhere to exposed collagen creating a clot, and the inflammatory phase begins with activation of platelets resulting in release of growth, bioactive, and hemostatic factors. Each factor plays a unique but codependent role in the early stages of the intrinsic and extrinsic pathways of the clotting cascade. Access to the wound site by neutrophils and macrophages occurs within hours of injury and likely serves to provide phagocytosis of tissue debris. Within a few days of injury, the proliferative phase begins that is characterized by angiogenesis, collagen deposition, granulation tissue formation, epithelialization, and wound contraction. Finally, spanning from several weeks to months after an injury, the remodeling phase involves collagen maturation and apoptosis of excess cells.
The potential benefits of PRP are thought to rely on the intrinsic properties and interplay between the concentrated growth factors [6–8, 18]. Some of these important growth factors include platelet-derived endothelial growth factor, transforming growth factor–β, vascular endothelial growth factor, fibroblast growth factor, epidermal growth factor, and insulin-like growth factor -1. The complex interactions of these growth and differentiation factors, along with adhesive protein factors such as fibronectin and vitronectin, are what is responsible for the healing response; promoting the long regenerative process of chemotaxis, cell proliferation, removal of tissue debris, angiogenesis, extracellular matrix formation, osteoid production, and collagen synthesis.
Preparation of PRP
Before the PRP injection, the patient is informed of the procedure and potential risks and benefits similar to other interventional procedures. Risks related to the interventional procedure include infection, hemorrhage, and soft-tissue injury. The use of sterile technique and a probe cover if using ultrasound guidance is warranted. In general, PRP is avoided when there are signs of local inflammation or infection or if there is a history of malignancy. The patient is also educated with regard to short-term and long-term expectations. Because the injection of PRP induces local inflammation, pain should be expected after the procedure. Nonsteroidal antiinflammatory drugs are also avoided 2 weeks prior and at least 2 weeks after the procedure so as to not inhibit the effects of growth factors and the healing response. Although the follow-up protocol may vary, physical therapy at least 2 weeks after the procedure is often considered.
The working definition of PRP is 1,000,000 per µL platelet count, which is five times the normal concentration found in whole blood. PRP is commonly prepared in the laboratory, operating suite, outpatient sports medicine clinic, or radiology setting using a centrifuge. There are different types of centrifuge methods: the gravitational platelet sequestration technique, which requires only a tabletop centrifuge system takes less than 30 minutes; the cell separator, which generally requires a full unit of whole blood; and smaller compact office systems. Centrifuge systems may differ in the ability to separate RBCs from platelets affecting concentration, separating leukocytes from platelets, or shearing platelets during the centrifugation process leading to premature platelet activation and degranulation. Standardizing the concentration and composition of PRP is difficult with such variability in the centrifugation market. No study, to our knowledge, has compared the effectiveness of different PRP preparation systems or platelet concentrations against one another for any indication.
Preparation of PRP begins with venipuncture and subsequent collection of a product-specific volume of autologous whole blood from the patient into a syringe containing an anticoagulant, typically at the point of care. Centrifugation separates the whole blood into three layers: RBCs (bottom layer, specific gravity = 1.09), platelet-poor plasma (top layer, specific gravity = 1.03), and platelet concentrate that contains WBCs (middle layer, specific gravity = 1.06). Typically the RBC layer is discarded after the first spin and a second spin yields a more concentrated platelet layer. The PRP amount is approximately 10% of the volume of whole blood originally collected; about 3 mL of PRP can be collected from 30 mL of whole blood after a 15-minute spin at 3,200 revolutions per minute. Once prepared, the PRP is maintained in a sterile environment and immediately used during an outpatient procedure or surgery. PRP is typically administered with a syringe through a 20- or 22-gauge needle either under ultrasound guidance or using anatomic landmark guidance in the clinic. The needle-induced bleeding during injection provides the clotting factor thrombin needed to activate platelets. Needle fenestration of the tendon may also be considered before the PRP injection. Exposure to collagen within the tissue further activates platelets. Bovine thrombin, calcium, or soluble type-I collagen have also been used to activate platelets but usually in the intraoperative setting. Typically, the use of local anesthetic in the region of the PRP injection is avoided because the effect on PRP success is not clear.
Four categories of platelet concentrate preparation are recognized: leukocyte-poor or pure platelet-rich plasma, leukocyte platelet-rich plasma, pure platelet-rich fibrin clot, and leukocyte platelet-rich fibrin clot. Factors such as centrifugation force and duration of centrifugation can yield different platelet concentration levels and composition. However, each has different biologic effects and potential uses. To our knowledge, no evidence-based classification scheme or guidelines specifying optimal use has been reported.
In Vitro and Animal Studies Using PRP
The first published in vitro study showed that PRP stimulated the proliferation of cell types such as osteoblasts, fibroblasts, tenocytes, chondrocytes, and mesenchymal stem cells. Lucarelli and colleagues showed that PRP had a positive effect on human stem cell proliferation and markedly increased cell numbers with increasing PRP concentration from 1% to 10%. Another in vitro study of cultured human tenocytes showed that PRP promoted tendon regeneration by inducing proliferation and total collagen production. However, other in vitro studies have reported contrasting results. The ability of PRP to differentiate cell lines is also controversial. One study showed that PRP can stimulate stem cell differentiation into osteoblasts, but others had mixed results.
Several animal studies using PRP have produced promising results. Bone healing was enhanced with respect to stronger callus formation in rabbit calvaria defects and in mandibular reconstruction in goats. The mechanism, according to Tomoyasu and colleagues, may be from a positive effect of PRP on osteoblastic differentiation.
Animal studies have also shown a positive effect on tendon healing. PRP injected into rat patellar tendons was found to be safe and had the potential of increasing early tendon healing activity by stimulating type I and III collagen required for repair and remodeling of tendons. However, other animal studies have shown contrasting results. Aghaloo and colleagues found no significant difference in bone graft strength between autogenous rabbit bone, PRP alone, or autogenous rabbit bone and PRP combined. Chaput and colleagues showed that PRP did not play a significant role in increasing bone ingrowth of PRP-treated implants in the distal femur of rabbits. Further investigation is needed using standardized PRP concentration and composition to help clarify biologic effects using animal models.
Clinical Studies Using PRP
Common musculoskeletal injuries account for nearly 100 million office visits annually in primary care and orthopedic clinic settings in the United States. PRP is seen by many orthopedic, primary care, and sports medicine physicians as a new treatment option for tendon, muscle, and bone injuries. Radiology clinics, especially those offering musculoskeletal ultrasound services in a collaborative sports medicine environment, are seeing significant increases in the volume of ultrasound-guided treatments for chronic tendinopathies, plantar fasciitis, and acute ligamentous and muscle injuries.
Clinical studies have reported that PRP use can shorten recovery time, enhance bone strength, produce bone healing in a shorter time, decrease the wound infection rate, and reduce surgery-related swelling and pain. However, most of these have been small nonrandomized studies or anecdotal case reports. The popularity and increased use of PRP is outpacing available scientific evidence; its use has especially increased after receiving media attention for its use in a professional athlete whose accelerated return to play in the Super Bowl was credited to PRP treatment.
An early clinical application of PRP was adding autologous fibrin made from concentrated platelets to cancellous bone during maxillofacial reconstructive surgery. Serial radiographic examinations showed consolidation of the bone at 4 weeks opposed to 8 weeks in control subjects, which was attributed to platelet enhancement of osteoconduction. Further studies detailing the clinical applications of PRP besides maxillofacial surgery have also included plastic surgery, heart bypass surgery, dermatology, and orthopedics. The clinical applications are also starting to permeate radiology practices associated with sports medicine clinics. PRP injections are now commonly used to treat chronic tendinopathies, including lateral epicondylosis (tennis elbow), plantar fasciitis, and Achilles and patellar tendinopathies. Onsite sports medicine clinics are also offering PRP treatments for acute injuries such as acute muscle tears, medial collateral ligament tears, and ankle sprains. A growing number of prospective randomized controlled trials have assessed the effects of PRP.
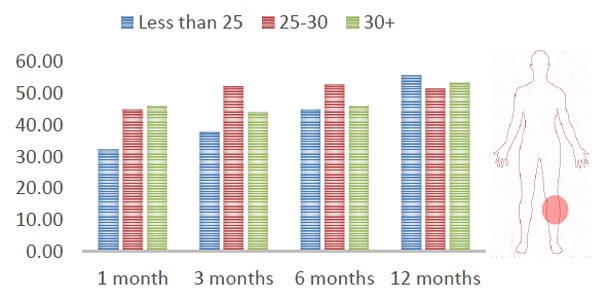
Tennis Elbow
Lateral epicondylosis is commonly referred to as “tennis elbow.” It is the most common cause of elbow pain in skeletally mature athletes, occurring in more than 50% of tennis players and resulting in weakness, pain, and suboptimal performance in athletes. It is characterized as repetitive microtrauma with mucoid degeneration of the common extensor tendon where it attaches to the lateral epicondyle of the humerus. Ultrasound is useful in evaluating lateral elbow pain, especially in helping to evaluate the extent of tissue damage in patients refractory to conservative management. A pathologic tendon may show hypoechogenicity, an increase in caliber, fibrillar disruption, or hyperemia on Doppler evaluation. Using clinical outcome measures, Mishra et al. reported in a small (n = 15) randomized clinical trial of PRP treatment for chronic elbow tendinosis that subjects receiving PRP in a single injection session had an 81% improvement in pain scores at 6 months and up to 93% at 25 months compared with their baseline status. A recent larger double-blind randomized controlled trial (n = 100) comparing PRP with corticosteroid injections found a statistically and clinically significant difference in disease specific quality of life in pain scores favoring the PRP group. Interestingly, the PRP group progressively improved at 1 year compared with the steroid group, which declined after an initial short-term improvement, suggesting that progressive healing may be responsible for clinical improvement in the PRP subjects. However, ultrasound evaluation was not used in either study, so tissue-specific healing is not known. Research involving imaging studies will help to confirm disease-specific tissue healing. Diagnostic imaging before PRP treatment will also help confirm the clinical diagnosis and establish baseline findings. In addition, ultrasound guidance for PRP treatments will ensure precise targeting of diseased tissue.
Achilles Tendinopathy
Chronic Achilles tendinopathy is a common overuse injury characterized by degeneration and abnormal tissue repair that affects athletes and middle-aged individuals. Achilles tendinopathy can progress to debilitating pain with significant health and economic cost to society. There is generally no effective definitive nonsurgical treatment; and 25–45% eventually require surgery, significantly adding to the cost and morbidity. PRP injections may offer a treatment option although current trials are limited. In a study comparing PRP to blinded sham saline injections, de Vos and colleagues reported significant improvement in both saline and PRP groups that slightly favored the PRP subjects but not by a statistically significant margin. However, the study was limited by a short follow-up period (24 weeks) and small sample size (n = 27) and was confounded by eccentric exercise performed in both groups, which has been reported to be an effective treatment of Achilles tendinopathy. Saline injection may not be the best placebo because it is likely active for tendinopathy; injecting saline into the tendon alters the pressure–volume relationship in a given space, thereby disrupting pathologic vascular and neural ingrowth, and injection-related needle trauma produces local bleeding, which is a known irritant and recruiter of platelets in both groups. One study suggested that dry needling, or percutaneous tenotomy, may be an effective alternative for treating chronic tendinopathy, including Achilles tendinopathy.
Plantar Fasciitis
Plantar fasciitis is a musculoskeletal disorder affecting the fascial enthesis and is the most common cause of inferior heel pain. Plantar fasciitis is an important cause of pain and disability among athletes but also is prevalent in the general population, especially sedentary individuals, affecting an estimated two million Americans annually. The cause of chronic plantar fasciitis may relate to a chronic degenerative condition from repetitive stress injury. These degenerative features are comparable to the tendinosis seen in tennis elbow, Achilles tendinopathy, and patellar tendon (Jumper’s knee). Currently, there is no uniformly effective treatment of plantar fasciitis, and no conventional therapy directly addresses the underlying pathophysiology of the degenerative tissue. Again, patients who have failed conservative management may be ideal candidates for PRP therapy, possibly circumventing the need for surgery.
Barrett and Erredge reported complete resolution of symptoms at 1 year in approximately 78% of subjects with plantar fasciitis treated with PRP. However, the study was limited by a small sample size and lack of a control group. Larger-scale randomized controlled studies are needed to help elucidate PRP as a viable treatment of this common musculoskeletal injury.
Postprocedure care data are limited and without standardization. Typically, after PRP treatment patients are kept nonweightbearing for 48 hours and in a weightbearing boot for 2 weeks with a gradual return to activity over the course of 6–8 weeks. However, some studies have shown a benefit to early rehabilitation with early stretching exercise to mechanically induce healing. Mechanical stimulation in one study of repaired animal tendons resulted in an increase force to failure. This increased strength was attributed to PRP effects allowing mechanical stimulation earlier in the healing process, thereby increasing the growth rate of tendon regeneration. Standardized postprocedure protocols for the various musculoskeletal conditions treated with PRP need to be established.
Acute Ligament Injuries
Despite limited evidence, PRP use for acute musculoskeletal injuries has also continued to gain popularity. In a recent review, Foster and colleagues discussed an unpublished retrospective study involving professional soccer players with grade 2 acute medial collateral ligament injuries showing an accelerated return to play by 27% in the PRP treated group compared with a control group treated with standard rest and rehabilitation. Here too, the sample size was small (n = 22). Similarly, a pilot study by Frei and colleagues described the use of calcium-activated PRP for type 3 ankle syndesmotic injuries in 11 patients. Investigators found an average time of healing of 5.18 weeks, with five patients achieving a full recovery without residual instability at 4 weeks, which differed from previously published reports showing an average return to play of 8 weeks after conservative standard of care treatment. Despite the small sample size, lack of imaging guidance, and absence of a control group, these early results suggest PRP may have an effect on augmenting ligament healing and reducing dynamic instability. Ultrasound guidance can offer precise needle placement for ligament injuries and monitor healing, which adds value to both the patient and clinical colleagues.
Acute Muscle Injuries
Acute muscle injuries (strains) are common athletic injuries, especially among elite athletes. The mechanism of injury is usually a direct blow to the muscle or from uncompensated eccentric loading during muscle contraction. Muscle strains of the thigh were the most common diagnosis (16%) in a survey study of the 2007 International Association of Athletics Federation World Championships. Other common muscle group injuries include gastrocnemius and quadriceps. Characterizing the severity of muscle injury by size and location is important, and imaging can play a vital role in prescribing treatment, monitoring rehabilitation, and stratifying risk for reinjury. The risk of reinjury is high. For example, there is a 30% reinjury rate within 1 year of initial hamstring injuries.
Preliminary clinical data supporting the use of PRP for acute muscle injuries includes work by Cugat et al. (presented at the 2005 meeting of the International Society of Arthroscopy, Knee Surgery, and Orthopedic Sports Medicine) who found a quicker return to play by up to 50% in those treated with PRP under direct ultrasound guidance after aspiration of the hematoma. Follow-up clinical and sonographic outcome measures documented progressive healing of the injured muscle. However, the study had a small sample size, was retrospective, and compared with previously published data on return to play instead of a control group. Validation of the potential role of PRP as an adjunct to standard rest, ice, compression, and elevation therapy will require further well-designed studies.
Discussion
Musculoskeletal injuries are prevalent among both athletes and sedentary individuals. Although most heal with conservative care, a substantial percentage of injuries are refractory to conservative care. Given the vast array of musculoskeletal injuries seen in daily practices, lack of consensus regarding standard treatment, and high cost to patients and society in loss of quality of life and absenteeism from work and sport, any promising advancements in minimally invasive therapies, such as PRP, deserve consideration and thorough investigation. Although PRP therapy has been in existence for the past 20 years, it has only recently been popularized in the United States, in part from extensive media attention. Many PRP studies have shown promising results for augmenting the natural healing response capable of producing stronger bone, regenerating tendon and muscle, and increasing the vascularity of tissue, all in a shorter time period. However, a definitive statement regarding appropriate indications cannot be made because studies are few and have often been limited by methodologic shortcomings. The most recent randomized controlled trials suggest that PRP is a promising therapy for chronic tendinopathy, a broad category of injuries with shared underlying pathophysiology.
Tendinopathy likely occurs from chronic repetitive stress in an area of relative hypovascularity. Unlike the acute inflammatory phase, the vast majority of overuse chronic musculoskeletal conditions, such as tennis elbow, Achilles tendinopathy, and plantar fasciitis, show no histopathologic evidence of inflammatory cells. No consensus about best treatment exists and no conventional therapy directly addresses the underlying pathophysiology of degenerative tissue. The proposed mechanism of action of PRP, assisting the natural healing response at the tissue level through augmented platelets and subsequent growth factors, may disrupt the vicious cycle of tendinopathy and allow normal healing to progress. PRP may be even more effective for acute injuries, such as muscle tears, medial collateral ligament and ankle sprains, and acute hamstring injuries. Such injuries are extremely common in sports and account for significant time lost and cost to society. These injuries are often slow to heal and are prone to reinjury. These acute injuries are often treated at the sports medicine complex or even in the athletic facility. PRP is well positioned as a potential acute-phase therapy because the centrifugation system is portable and easy to use and preparation of PRP is quick with very minimal risk. Current studies have not reported any complications with PRP use.
Investigators also advocate the use of ultrasound-guidance to ensure precise needle placement as well as real-time visualization of the needle during fenestration in preparing the injection site. In addition, areas of neovascularization of inflammation can be specifically targeted during Doppler interrogation of the diseased tissue. MRI or ultrasound can also be used to monitor the healing effects of PRP-treated diseased tissue and should be used in future research studies to document changes in tissue morphology and structure after PRP therapy. Studies involving ultrasound have reported a decrease in thickness and cross-sectional area and normalization of the hypoechogenic portions of the tendon after treatment. In hamstring injuries, MRI plays an important role in characterizing severity of muscle injury by size and location to help stratify treatment options, monitor healing during rehabilitation, and prescribe risk for reinjury.
Other PRP studies have had contradictory results. Some animal and clinical studies have shown no benefit with PRP use. However, critics state that these studies were conducted without a standard PRP dose and possibly inadequate concentration levels. Some investigators have argued that the composition of PRP, such as leukocyte-rich or leukocyte-poor PRP, may lead to different healing responses. Nevertheless, larger-scale randomized controlled trials are needed before PRP can be adopted as a mainstream treatment. Both basic science and clinical research designed to help develop a standard PRP concentration, dose, and composition would help clarify the current mixed results found in the literature. In addition, developing a standard postprocedure protocol that involves short-term immobilization followed by appropriate rehabilitation may also be important in promoting rather than inhibiting the healing effects of PRP.
Research Direction
Despite our current understanding of the healing process, complete knowledge of the complex codependent biologic properties of PRP is largely unknown, and there is yet much to be understood of the clinical effects of its various applications. Future basic science research should address the biologic activity of PRP in various wound environments. For example, what is the optimum concentration of PRP to maximize healing? Is there an inhibitory concentration level? Does the PRP remain within the tendon or muscle injected? Is PRP as effective in the acute setting as it seems to be in the chronic tendinopathy setting? Is the mechanism of action similar in each setting? When is the best time to treat an acute injury of muscle, tendon, or ligament? What is the optimal PRP composition and injection protocol? How important is tendon fenestration or tenotomy in conjunction with PRP? And lastly, a preliminary study showed that efficacy of PRP may be pH-dependent, which may be seen in different wound environments and needs further investigation.
Basic science research for elucidating optimal PRP concentration and composition are needed. Most studies involving PRP have not used a standard protocol of centrifugation, platelet activation, or PRP composition. For example, the leukocyte component of PRP has not been fully studied. Some authors recommend removing leukocytes to make a more pure PRP concentrate, without clear supporting evidence. Leukocytes have been shown to release oxygen-free radicals and may result in secondary tissue damage in the setting of muscle injuries. However, several recent studies have suggested the importance of keeping leukocytes in the PRP concentrate. Leukocytes may provide an antiinfectious environment, promote vascular endothelial growth factor, and regulate immunity. Leukocyte use in PRP has also decreased wound infection rates and did not adversely affect outcomes of PRP use in joint surgery. Recent studies have shown that leukocyte use in PRP is able to promote the regenerating and remodeling process in tendons. Further studies are needed to help differentiate the individual and synergistic effects of platelets and leukocytes to optimize the PRP composition and utility of various platelet-rich preparations.
No evidence-based classification scheme or guidelines specifying optimal use of PRP have been reported. Establishing a classification scheme for the different platelet preparations will help guide further investigations in optimizing an effective platelet concentration and composition.
Billing and Reimbursement Issues
An additional issue with regard to the use of PRP is related to billing and the potential lack of reimbursement for the procedure. The Current Procedural Terminology code for PRP injection, which was implemented July 1, 2010, is 0232 T (Injection[s], platelet-rich plasma, any tissue, including image guidance, harvesting, and preparation when performed). This category 3 code is a temporary code used for emerging technologies, services, and procedures that allows data collection to be used to document widespread usage for Food and Drug Administration approval. Patients must be made aware that a PRP injection may not be fully reimbursed and ultimately they may be held responsible for payment of the procedure. It should be noted that the 0232 T billing code also includes imaging guidance, harvesting, and preparation; therefore, these aspects of the procedure cannot be billed separately. Establishment of this temporary billing code creates problems when attempting to provide patient care; however, this also emphasizes the importance of further research to provide additional information with regard to the potential effectiveness of PRP so that a permanent code can be established.
Conclusion
The application of a promising treatment method for musculoskeletal injuries is always met with considerable enthusiasm, often outpacing basic science and clinical studies. A growing number of orthopedic surgeons and sports medicine physicians are using PRP and are eager to establish its mainstream presence, which has spilled over to radiology practices that can offer MRI or ultrasound assessment of soft-tissue injuries and guide treatment. However, enthusiasm does not replace scientific evidence. The potential role of PRP in healing musculoskeletal injuries, especially in the high-level athlete, is an exciting frontier that may even lead to newer improved therapies, but a healthy amount of caution should be maintained until clinical evidence is established. Further studies are needed to establish effectiveness, indications, and protocols for PRP application in the treatment of musculoskeletal injuries.
Contributing Physicians; Kenneth S. Lee, John J. Wilson, David P. Rabago, Geoffrey S. Baer, Jon A. Jacobson and Camilo G. Borrero