Jan 2, 2014 | Hip, Osteoarthritis, Stem Cell Procedures
An orthopedic surgeon recently compared patients suffering from hip arthritis, where he performed traditional hip replacement surgery on one group and used the latest stem cell treatment on another group. He found that the patients receiving stem cell treatments experienced more range of motion a year after receiving treatment than patients receiving hip replacement surgery. He also found that 73% of the patients that received the stem cell treatment were able to return to sporting activities. In terms of overall functional scores, patients receiving stem treatments were very similar to the surgery group, with the surgery group receiving a slightly better score for pain management[1]. However, when you compare the invasiveness of surgery to stem cell therapy, the advantages of stem cell treatments are striking.
Traditional surgery: What are the risks?
Traditional hip surgery can range from removing the ball of the femur and replacing it with a metal ball to a total hip replacement. With a complete hip replacement, the entire head of the femur is removed and a metal prosthesis is hammered into place on the hip bone as well as the socket on the pelvis. Risks with these types of surgical procedures include:
- Risk of infection
- Increased risk of stroke and heart attack
- Allergic reaction to the metal used in the implant
- Wear particles from the implant causing high levels of metal ions in the blood stream
- Risk of blood clots in the legs (DVT) and/or lungs (PE)
- Painful post-surgical recovery
- Prolonged rehabilitation
- Recurrent hip dislocations if the replacement is not placed properly
- Failure of the hip prosthesis
After a hip replacement, the materials involved wear down over time, meaning that a hip revision surgery might be required at some point to replace failing implants. This surgery can be longer and even more involved that the original procedure.
Biologic regenerative treatments, such as Stem Cell Therapy, are much less invasive procedures with a quicker return to normal daily activity when compared to surgery. To maximize healing, Stem Cell treatments are used with other leading treatments in the field including Prolotherapy, Platelet Rich Plasma (PRP) and Platelet Lysate therapy. In certain cases, a patient’s unique medical condition or circumstance may preclude utilizing the benefits of all treatments used together. In this case, a customized plan is developed using one or more of the treatments to obtain the best patient outcomes possible. While sometimes there is no good alternative to surgical repair, most often biologic repair offers a better option.
Stem Cell Therapy: The Process
Stem Cell therapy makes use of the supply of stem cells available in the body to help repair injured and degenerated tissues. The easiest place to harvest these stem cells is from the back of the hip area, under ultrasound or x-ray guidance. This harvesting procedure is well tolerated by patients and not considered difficult as many patients claim it is not painful.
After bone marrow blood is drawn, it is centrifuged to concentrate and purify the stem cells, with each stem cell specimen custom designed to meet the needs of the specific injury. Utilizing either fluoroscopy or ultrasound, the stem cells are placed on the injured site precisely to improve the likelihood that stem cells will adhere to the damaged area and promote healing. After the stem cells are placed, concentrated platelets and other adjuvants are injected to stimulate the stem cells to multiply, and then transform into the repair cells needed to regenerate new tissue. The platelets are injected again 2-5 days later to keep the stem cells activated and promote additional healing.
Prolotherapy
Injected 2-5 days before the stem cells, Prolotherapy contains a solution of concentrated dextrose and local anesthetic (steroids are not used). This solution stimulates the body’s natural ability to repair damaged tissue, encouraging new growth and creating a positive environment into which the stem cells are placed.
Platelet Rich Plasma
Platelets initiate tissue repair by releasing growth factors. These growth factors start the healing process by attracting cells that repair us including critical stem cells. Platelet Rich Plasma therapy intensifies this process by delivering a higher concentration of platelets. The therapy involves a small sample of the patient’s blood placed in a centrifuge to separate the platelets from the other blood components. The concentrated PRP is then injected into and around the point of injury, significantly strengthening the body’s natural healing. Our process for PRP is much different and sets us apart. Because our samples are all hand processed, we are able to produce PRP that is free of contaminating red and white cells, which can inhibit repair. This same special process also allows us to customize the concentration and volume for each individual and each injury type. This greatly improves outcomes.
Platelet Lysates
Platelets in the blood release powerful tissue growth factors that aid in the healing process. Normally this occurs slowly over time, but through the creation of a Platelet Lysate solution, a high concentration of growth factors can be released immediately into the body. The result is a targeted, faster healing process. Additionally, there are areas of the body where using traditional PRP may cause too much inflammation. Platelet Lysates are a better option where inflammation may become an issue.
While additional study is needed[2], the results of biologic regenerative treatments are too promising to ignore. This can be a real solution to alleviate the pain and loss of function from hip arthritis without the drastic approach of surgically cutting open a patient to replace the entire hip.
[1] Mitchell, B. Sheinkop, MD, The Orthobiologic Institute, “BMAC Intervention Versus Joint Arthroplasty for Arthritis,” results presented to LA Orthobiologic Conference on June 7th, 2013; http://www.regenexx.com/wp-content/uploads/2013/06/11-MITCHELL-B-SHEINKOP1.pdf
[2] It should be noted in the Sheinkop study that this was a comparison of patients treated in 2007 with surgery and patients treated in 2011-13 with stem cells. It was not a randomized controlled trial, as that type of study has not yet been conducted for stem cell treatments. It should also be noted that Dr. Sheinkop is a member of the Chicago Regenexx Network, Regenexx is the same treatment offered by Stem Cell Arts.

Jan 2, 2014 | Prolotherapy, PRP, Shoulder / Rotator Cuff, Stem Cell Procedures

Stem cell and platelet procedures can be used to help heal rotator cuff injuries and degenerative shoulder conditions
Recent Studies cited by the American Academy of Orthopaedic Surgeons show the potential benefits of regenerative treatments such as Stem Cell therapy and Platelet Rich Plasma (PRP) [1]. Also, a recent case history cited a patient with a severely debilitating rotator cuff injury—a case where the patient was going to lose her job due to the injury—experiencing a 90% improvement in rotator cuff pain, function and mobility after approximately 7 months of treatment[2]. While this example may be above normal expected results, it is indicative of just how far these treatments have come in healing this type of injury.
Surgery is a common treatment option following a rotator cuff injury. But according to the American Academy of Orthopaedic Surgeons, possible complications of surgery include nerve injury, infection, deltoid detachment, permanent stiffness or loss of motion and a re-tear of the tendon.[3] The advantage of regenerative treatment is that they are minimally invasive compared to surgery, and they have the ability to actually heal the injury without scalpels, and the physical stitching together of tendons and tissue.
[accordion title=”Most Commonly Treated Shoulder Conditions:” is_open=”no”]
Below is a list of the most common shoulder and rotator cuff injuries and conditions that we treat with stem cells or platelet procedures. This is not an all-inclusive list.
- Rotator cuff tears
- AC Joint Separation
- Arthritis of the shoulder joint
- Labral tears or degeneration
- Thoracic outlet syndrome
- Rotator cuff tendonitis
- Recurrent shoulder dislocations
[/accordion]
To maximize healing, Stem Cell treatments are used with other leading treatments in the field including Prolotherapy, Platelet Rich Plasma (PRP) and Platelet Lysate therapy. In certain cases, a patient’s unique medical condition or circumstance may preclude utilizing the benefits of all treatments used together. In this case, a customized plan is developed using one or more of the treatments to obtain the best patient outcomes possible. While sometimes there is no good alternative to surgical repair, most often biologic repair offers a better option.
Video: Treating the Shoulder and Rotator Cuff Non-Surgically with Regenerative Biologic Treatments:
[youtube id=”lLGP74H7EHc” width=”600″ height=”350″]
Stem Cell Therapy: The Process
Stem Cell therapy makes use of the supply of stem cells available in the body to help repair injured and degenerated tissues. The easiest place to harvest these stem cells is from the back of the hip area, under ultrasound or x-ray guidance. This harvesting procedure is well tolerated by patients and not considered difficult as many patients claim it is not painful.
After bone marrow blood is drawn, it is centrifuged to concentrate and purify the stem cells, with each stem cell specimen custom designed to meet the needs of the specific injury. Utilizing either fluoroscopy or ultrasound, the stem cells are placed on the injured site precisely to improve the likelihood that stem cells will adhere to the damaged area and promote healing. After the stem cells are placed, concentrated platelets and other adjuvants are injected to stimulate the stem cells to multiply, and then transform into the repair cells needed to regenerate new tendon. The platelets are injected again 2-5 days later to keep the stem cells activated and promote additional healing.
Prolotherapy
Injected 2-5 days before the stem cells, Prolotherapy contains a solution of concentrated dextrose and local anesthetic (steroids are not used). This solution stimulates the body’s natural ability to repair damaged tissue, encouraging new growth and creating a positive environment into which the stem cells are placed.
Platelet Rich Plasma
Platelets initiate tissue repair by releasing growth factors. These growth factors start the healing process by attracting cells that repair us including critical stem cells. Platelet Rich Plasma therapy intensifies this process by delivering a higher concentration of platelets. The therapy involves a small sample of the patient’s blood placed in a centrifuge to separate the platelets from the other blood components. The concentrated PRP is then injected into and around the point of injury, significantly strengthening the body’s natural healing. Our process for PRP is much different and sets us apart. Because our samples are all hand processed, we are able to produce PRP that is free of contaminating red and white cells, which can inhibit repair. This same special process also allows us to customize the concentration and volume for each individual and each injury type. This greatly improves outcomes.
Platelet Lysates
Platelets in the blood release powerful tissue growth factors that aid in the healing process. Normally this occurs slowly over time, but through the creation of a Platelet Lysate solution, a high concentration of growth factors can be released immediately into the body. The result is a targeted, faster healing process. Additionally, there are areas of the body where using traditional PRP may cause too much inflammation. Platelet Lysates are a better option where inflammation may become an issue.
Regenerative Treatments Deliver Solid Results
In the case history mentioned above, the patient previously tried cortisone injections, acupuncture, physical therapy and taking 2400mg of Ibuprofen daily. The result was that her pain consistently intensified. After losing range of motion in her shoulder, she developed pain and muscle spasms in her neck. She felt that she was unable to continue her career or participate in sports. After receiving regenerative care, she experienced 60-70% improvement in overall pain function and mobility after just 5 months. Two months later, this number jumped to 90%[4]. Regenerative biologic treatment is a real solution to negate the effects of a rotator cuff injury without the risks associated with more invasive surgical procedures, and can finally bring relief to a patient where other treatments have failed.
[1] T. Sean Lynch, MD, “The Role of Biologics in Rotator Cuff Repairs,” AAOSNow; August 2013; Volume 7, Number 8; American Academy of Orthopaedic Surgeons (AAOS); http://www.aaos.org/news/aaosnow/nov11/clinical3.asp
[1] Donna D. Alderman, DO, Sean C. Robbins, BA, “Platelet Rich Plasma Prolotherapy for Rotator Cuff Tears,” Practical Pain Management, September 2012; 21-23
[1] “Rotator Cuff Tears: Surgical Treatment Options,” OrthoInfo; American Academy of Orthopaedic Surgeons (AAOS); http://orthoinfo.aaos.org/topic.cfm?topic=A00406
[1] Donna D. Alderman, DO, Sean C. Robbins, BA, “Platelet Rich Plasma Prolotherapy for Rotator Cuff Tears,” Practical Pain Management, September 2012; 21-23
Jan 2, 2014 | Knee, Prolotherapy, PRP, Stem Cell Procedures
A recent clinical study found that Regenerative Injection Therapy (RIT) delivered significant improvement in knee function and pain to those suffering from knee osteoarthritis. The study found that study participants receiving RIT treatment experienced an 29.5% improvement in knee pain, stiffness and function measured according to the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC score).[1]
This treatment is just one of many new options available in the fight against knee osteoarthritis. Osteoarthritis of the knee usually occurs in knees that have experienced trauma, infection, or injury. The articular cartilage, which acts as a protective cushion, begins to deteriorate. What these new biological treatments accomplish is assisting and stimulating the growth of new cartilage. It’s an approach that does not simply mask the symptoms, but addresses the root cause of the condition.
[youtube id=”4ZcfslvNPJA” width=”600″ height=”350″]
To maximize healing, Stem Cell treatments are used with other leading treatments in the field including Prolotherapy, Platelet Rich Plasma (PRP) and Platelet Lysate therapy. In certain cases, a patient’s unique medical condition or circumstance may preclude utilizing the benefits of all treatments used together. In this case, a customized plan is developed using one or more of the treatments to obtain the best patient outcomes possible. While sometimes there is no good alternative to surgical repair, most often biologic repair offers a better option.
Stem Cell Therapy: The Process
Stem Cell Therapy makes use of the supply of stem cells available in the body to help repair injured and degenerated tissues. The easiest place to harvest these stem cells is from the back of the hip area, under ultrasound or x-ray guidance. This harvesting procedure is well tolerated by patients and not considered difficult as many patients claim it is not painful.
After bone marrow blood is drawn, it is centrifuged to concentrate and purify the stem cells, with each stem cell specimen custom designed to meet the needs of the specific injury. Utilizing either fluoroscopy or ultrasound, the stem cells are placed on the injured site precisely to improve the likelihood that stem cells will adhere to the damaged area and promote healing. After the stem cells are placed, concentrated platelets and other adjuvants are injected to stimulate the stem cells to multiply, and then transform into the repair cells needed to regenerate new cartilage. The platelets are injected again 2-5 days later to keep the stem cells activated and promote additional healing.
Prolotherapy
With Prolotherapy, a solution of concentrated dextrose and local anesthetic (steroids are not used) stimulates the body’s natural ability to repair the cartilage, encouraging new growth and creating a positive environment into which the stem cells are placed. Prolotherapy treatments are usually scheduled every two to six weeks until the cartilage is regenerated.
Platelet Rich Plasma
Platelets initiate tissue repair by releasing growth factors. These growth factors start the healing process by attracting cells that repair us including critical stem cells. Platelet Rich Plasma therapy intensifies this process by delivering a higher concentration of platelets. The therapy involves a small sample of the patient’s blood placed in a centrifuge to separate the platelets from the other blood components. The concentrated PRP is then injected into and around the point of injury, significantly strengthening the body’s natural healing. Our process for PRP is much different and sets us apart. Because our samples are all hand processed, we are able to produce PRP that is free of contaminating red and white cells, which can inhibit repair. This same special process also allows us to customize the concentration and volume for each individual and each injury type. This greatly improves outcomes.
Platelet Lysates
Platelets in the blood release powerful tissue growth factors that aid in the healing process. Normally this occurs slowly over time, but through the creation of a Platelet Lysate solution, a high concentration of growth factors can be released immediately into the body. The result is a targeted, faster healing process. Additionally, there are areas of the body where using traditional PRP may cause too much inflammation. Platelet Lysates are a better option where inflammation may become an issue.
A Real Solution to Regain Knee Function
These regenerative treatments are a promising revolution in the treatment of knee osteoarthritis. While not a “cure,” these treatments can slow the progression of the disease, significantly reduce pain and restore knee function and mobility to the patient. When combined with short term knee bracing and physical therapy, the effects of this approach can be greatly magnified even further to restore quality of life to most patients.
[1] Richard Dumais, MD, Catherine Benoit, MD, Alex Dumais, MD, Lise Babin, MD, Rachel Bordage, BScN, Claire de Arcos, BScPT, Jacques Allard, PhD, Mathieu Bélanger, PhD, “Effect of Regenerative Injection Therapy on Function and Pain in Patients with Knee Osteoarthritis: A Randomized Crossover Study,” Pain Medicine 2012; 13; 990-999; Wiley Periodicals, Inc.
Jan 2, 2014 | Knee, Prolotherapy, PRP, Stem Cell Procedures
According to a study published in the American Journal of Sports Medicine, out of 295 knee surgeries for Meniscus repair that occurred over a 9-year period, 37 needed subsequent surgeries to correct a failed repair. After a review of medical literature, the study found that the failure rate for this type of surgery could range anywhere from 5-45%[1].
One of the problems with this type of surgery is that when trying to repair these tears, surgeons are often removing Meniscus tissue surrounding the tear. The reason is if the location of the Meniscus tear is on the interior of the knee, the lack of proximity to a blood supply means that the tear may not heal properly. This approach unfortunately can lead to complications including increased arthritis in the knee in the future.
The Meniscus is living tissue acting as a shock absorber in the knee, which is why biologic regenerative treatments hold such promise to actually heal the injury instead of attempting to carve it out. The result is a less invasive procedure, with a quicker return to normal daily activity when compared to surgery. To maximize healing, Stem Cell treatments are used with other leading treatments in the field including Prolotherapy, Platelet Rich Plasma (PRP) and Platelet Lysate therapy. In certain cases, a patient’s unique medical condition or circumstance may preclude utilizing the benefits of all treatments used together. In this case, a customized plan is developed using one or more of the treatments to obtain the best patient outcomes possible. While sometimes there is no good alternative to surgical repair, most often biologic repair offers a better option.
Stem Cell Therapy
Stem Cell therapy makes use of the supply of stem cells available in the body to help repair injured and degenerated tissues. The easiest place to harvest these stem cells is from the back of the hip area, under ultrasound or x-ray guidance. This harvesting procedure is well tolerated by patients and not considered difficult as many patients claim it is not painful.
After bone marrow blood is drawn, it is centrifuged to concentrate and purify the stem cells, with each stem cell specimen custom designed to meet the needs of the specific injury. Utilizing either fluoroscopy or ultrasound, the stem cells are placed on the injured site precisely to improve the likelihood that stem cells will adhere to the damaged area and promote healing. After the stem cells are placed, concentrated platelets and other adjuvants are injected to stimulate the stem cells to multiply, and then transform into the repair cells needed to regenerate new tissue. The platelets are injected again 2-5 days later to keep the stem cells activated and promote additional healing.
Prolotherapy
Injected 2-5 days before the stem cells, Prolotherapy contains a solution of concentrated dextrose and local anesthetic (steroids are not used). This solution stimulates the body’s natural ability to repair damaged tissue, encouraging new growth and creating a positive environment into which the stem cells are placed.
Platelet Rich Plasma
Platelets initiate tissue repair by releasing growth factors. These growth factors start the healing process by attracting cells that repair us including the critical stem cells. Platelet Rich Plasma therapy intensifies this process by delivering a higher concentration of platelets. The therapy involves a small sample of the patient’s blood placed in a centrifuge to separate the platelets from the other blood components. The concentrated PRP is then injected into and around the point of injury, significantly strengthening the body’s natural healing. Our process for PRP is much different and sets us apart. Because our samples are all hand processed, we are able to produce PRP that is free of contaminating red and white cells, which can inhibit repair. This same special process also allows us to customize the concentration and volume for each individual and each injury type. This greatly improves outcomes.
Platelet Lysates
Platelets in the blood release powerful tissue growth factors that aid in the healing process. Normally this occurs slowly over time, but through the creation of a Platelet Lysate solution, a high concentration of growth factors can be released immediately into the body. The result is a targeted, faster healing process. Additionally, there are areas of the body where using traditional PRP may cause too much inflammation. Platelet Lysates are a better option where inflammation may become an issue.
Eliminate the Risks of Surgery
Another recent study demonstrated that a group of patients receiving stem cell treatment experienced double the pain relief compared to a control group in the study over a 2 year period. In particular, one physician from the Mayo clinic monitoring the study noted that there were no adverse events related to the treatment[2]. That fact alone makes biologic regenerative treatments a very attractive option to patients dealing with a Knee Meniscus tear.
[1] Nicolas Pujol, MD, Olivier Barbier, MD, Philippe Boisrenoult, MD and Philippe Beaufils, MD, “Amount of Meniscal Resection After Failed Meniscal Repair,” The American Journal of Sports Medicine; August 2011; vol. 39 no. 8; http://ajs.sagepub.com/content/39/8/1648.abstract
[2] John Gever, Senior Editor, MedPage Today, Reviewed by Zalman S. Agus, MD, Emeritus Professor
University of Pennsylvania School of Medicine and Dorothy Caputo, MA, RN, BC-ADM, CDE, Nurse Planner “Stem Cells Show Promise for Meniscal Tears,” MedPage Today; Feb 10, 2012; http://www.medpagetoday.com/MeetingCoverage/AAOS/31131
Nov 22, 2013 | Blog, Research, Stem Cell Procedures
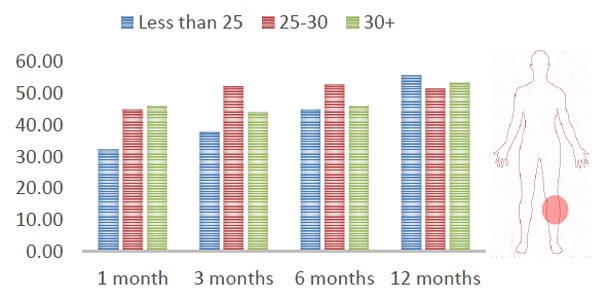
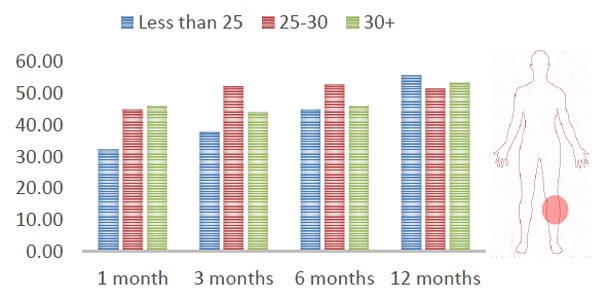
New Data out from Regenexx this week shows that BMI may not impact outcomes of stem cell procedures. The data is based on the Regenexx advanced treatment registry, which collects outcome information as patients are treated. Their biostatistician queried the database for Regenexx-SD (same-day) knee stem cell treatment patients vs. their Body Mass Index (BMI). BMI means the patient’s weight vs. their height. The current guidelines state that normal weight is a BMI of 18.5-25 and overweight is 25-30 and obese is >30.
BMI had previously been considered to be one factor that may produce different outcomes for an individual, but the new data shows that at 1 month, 3 month, 6 months and 12 month follow-ups after the procedure, there was no indication that a high BMI had any impact on a patient’s outcome.
Click here for a PDF infographic showing the BMI outcome comparisons.

Jun 25, 2013 | Stem Cell Procedures
The average athlete may soon have access to the benefits of stem cell research. Right away and now two months later Eli is back working out and lifting weights, as he never had the pain at all. “Within two days I was stronger than I’ve been in a dozen years.”
###
Source: http://abcnews.go.com